A New Era in Patient-Centered Therapy
Digital therapeutics and virtual rehabilitation are redefining how therapy is delivered, particularly for individuals managing chronic conditions and recovery. These solutions use software-based interventions, often powered by artificial intelligence (AI), to deliver evidence-based therapeutic programs that were once limited to physical clinics. With these innovations, healthcare providers can offer effective, personalized care that extends far beyond the traditional walls of a hospital or therapy center.
What Are Digital Therapeutics?
Digital therapeutics (DTx) are clinically validated, software-driven treatments designed to prevent, manage, or treat medical disorders and diseases. Unlike general wellness apps, DTx programs are prescribed by healthcare professionals and often go through clinical trials to demonstrate their efficacy. These platforms are regulated and often reimbursed similarly to traditional treatments, positioning them as integral parts of modern care plans.
Virtual Rehabilitation: Therapy Without Borders
Virtual rehabilitation refers to the remote delivery of therapeutic interventions using digital technologies. This includes physical therapy, occupational therapy, and cognitive training programs delivered via mobile apps, smart devices, and cloud-based systems. Patients receive guided exercises, real-time feedback, and ongoing progress assessments—without needing to travel to a clinic or hospital.
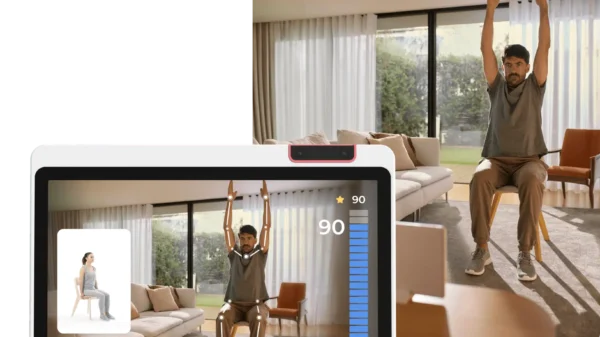
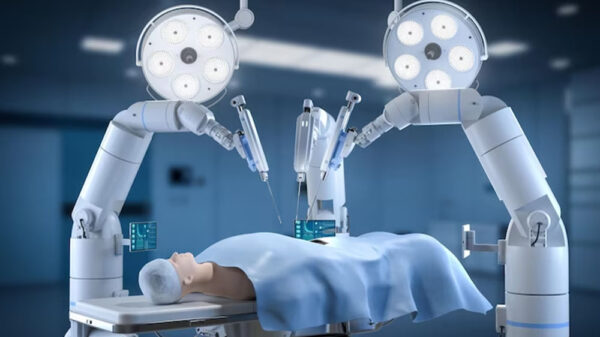
Sword Health and the Rise of AI-Driven Rehab
Companies like Sword Health are pioneering AI-powered virtual rehabilitation. Their platforms provide musculoskeletal (MSK) care through motion sensors, virtual physical therapists, and real-time feedback. These tools analyze a patient’s movement, adapt exercises accordingly, and offer personalized recommendations—mimicking the attention of an in-person therapist with added convenience and scale.
Addressing the Global Burden of MSK Conditions
Musculoskeletal disorders, including back pain, arthritis, and joint injuries, are among the leading causes of disability worldwide. Digital therapeutics offer scalable solutions to address these widespread conditions. With virtual rehab platforms, patients can begin therapy faster, follow structured treatment plans, and avoid delays caused by clinic scheduling or travel barriers.
Improving Patient Adherence and Outcomes
One of the key challenges in rehabilitation is patient adherence. Digital platforms increase engagement by using gamification, daily reminders, and progress tracking features. Patients can visualize their improvement, receive motivational feedback, and feel more in control of their recovery journey—ultimately leading to better clinical outcomes.
Real-Time Monitoring and Feedback
Unlike traditional rehab settings that require periodic in-person check-ins, virtual rehabilitation offers real-time monitoring. AI-powered systems track performance during each session, detect movement errors, and suggest immediate corrections. This continuous loop of feedback ensures that patients perform exercises safely and correctly, reducing the risk of further injury.
Reducing Healthcare Costs and Resource Use
Digital therapeutics reduce the financial burden on healthcare systems by minimizing the need for in-person appointments and hospital visits. For providers, this means fewer overhead costs; for patients, it means fewer travel expenses, time off work, and out-of-pocket therapy fees. This model is especially valuable for health systems facing resource constraints and workforce shortages.
Expanding Access in Underserved Communities
Virtual rehabilitation expands access to care in rural or underserved regions where physical therapy services may be limited or unavailable. All that’s required is a connected device, making it easier for patients in geographically isolated areas to receive consistent, high-quality care. This accessibility helps bridge the healthcare gap for populations with limited options.
Enhancing Continuity of Care
These platforms also support continuity of care by integrating with electronic health records and providing reports to healthcare providers. Physicians and therapists can track progress, adjust plans, and coordinate with other members of a care team—ensuring that patients receive holistic, well-managed treatment throughout their recovery process.
Regulatory Support and Clinical Validation
Digital therapeutic solutions are increasingly being validated through rigorous clinical trials and approved by regulatory bodies such as the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA). This regulatory backing enhances their credibility and ensures that patients receive therapies that are both safe and effective.
Mental Health Applications and Cognitive Rehab
While most known for physical therapy, digital therapeutics also support mental health and cognitive rehabilitation. Platforms are available to treat anxiety, depression, ADHD, and PTSD, using behavioral interventions delivered through mobile applications. Similarly, cognitive rehab tools help patients recover brain function after strokes or traumatic injuries through interactive exercises and brain training modules.
The Role of AI and Machine Learning
Artificial intelligence plays a pivotal role in optimizing virtual rehabilitation. Machine learning algorithms analyze large datasets to predict recovery timelines, adjust treatment intensity, and recommend personalized interventions. These dynamic adjustments ensure that therapy is responsive to the patient’s evolving needs.
Future Innovations and Integration with Wearables
The future of digital therapeutics lies in deeper integration with wearable technology. Smartbands, motion sensors, and connected devices can collect granular data on posture, mobility, and biometric feedback—feeding into AI platforms to make real-time treatment decisions. This combination will further refine virtual rehab and move toward even more personalized healthcare experiences.
Conclusion: Toward a Smarter Recovery Model
Digital therapeutics and virtual rehabilitation are more than just alternatives to in-person therapy—they represent a smarter, more scalable, and patient-centric approach to recovery and chronic care. By combining AI-driven personalization, real-time feedback, and accessibility, these tools are shaping a healthcare future where effective therapy is available anytime, anywhere.